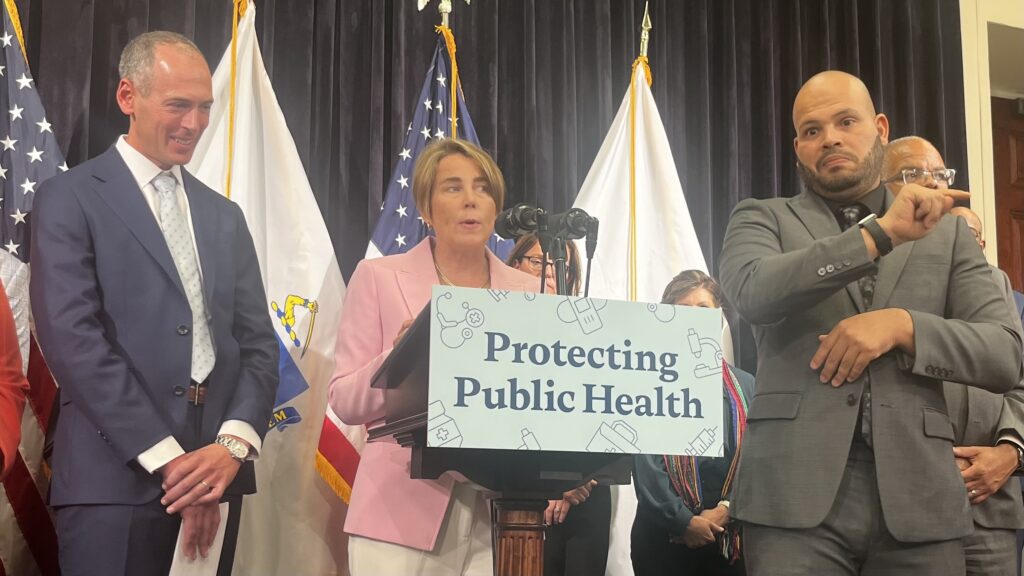
Massachusetts Orders Insurers: In a landmark move, Massachusetts has become the first U.S. state to mandate insurance coverage for vaccines backed by its state health department, even if the Centers for Disease Control and Prevention (CDC) issues narrower recommendations. Governor Maura Healey announced the order on September 4, 2025, underscoring her administration’s commitment to expanding vaccine access and protecting residents’ health.
Traditionally, insurers rely on CDC advisory panel recommendations to determine coverage for vaccines, especially those approved by the U.S. Food and Drug Administration (FDA). By decoupling coverage from federal guidance, Massachusetts has created a precedent that could reshape vaccine policy nationwide. The order ensures that residents won’t face insurance barriers, even if federal agencies scale back recommendations, as has recently happened with COVID-19 vaccines.
The announcement comes at a time of growing debate over federal vaccine policies under Health Secretary Robert F. Kennedy Jr., a longtime vaccine skeptic. In recent months, Kennedy has narrowed federal recommendations, particularly for COVID-19 shots, excluding many younger and healthy groups. Massachusetts’ decision is therefore not just a health policy shift, but also a direct response to what state leaders see as gaps in federal protections.
Highlights of Massachusetts’ Vaccine Coverage Order
- Mandatory Coverage Beyond CDC: Insurers must now cover any vaccine endorsed by the Massachusetts Department of Public Health (DPH).
- Expanded Pharmacy Role: Pharmacies are authorized to continue providing COVID-19 vaccines to residents aged five and above.
- State Oversight of Routine Vaccines: The DPH will determine which vaccines pharmacists can administer in Massachusetts.
- Regional Public Health Collaboration: Massachusetts will lead a Northeast alliance focused on vaccine policy, disease tracking, and emergency preparedness.
Why the Decision Matters Now
The move comes amid uncertainty over COVID-19 vaccine coverage in the U.S. The FDA recently limited approval of updated COVID-19 shots for those under 65 to people with health risks, sparking concerns about insurance gaps. Earlier in May, Kennedy said the U.S. would no longer recommend routine COVID-19 shots for healthy children and pregnant women, a stance that drew strong criticism from medical associations.
By stepping in, Massachusetts ensures continuity of vaccine access for its residents, regardless of federal rollbacks. Governor Healey emphasized that the policy is designed to protect public trust and prevent confusion:
“We are ensuring evidence-based, science-driven access to vaccines for all Massachusetts residents.”
National Landscape: States Taking Diverging Paths
Massachusetts’ decision adds to a growing patchwork of state-level vaccine policies:
- California, Oregon, Washington, and Hawaii: Formed a joint alliance to unify vaccine recommendations.
- Colorado: Announced it will act quickly to secure updated COVID-19 vaccines for all residents.
- Florida: Took the opposite route, announcing plans to eliminate all state vaccine mandates, including those required for schoolchildren.
This fragmentation highlights a shifting power balance in U.S. public health, where states are increasingly asserting independence from federal agencies.
Read about: Zero GST on Life & Health Insurance From September 22: Who Benefits and How?
Impact on Residents and Insurers
For residents, the benefits are clear: no matter what the CDC recommends, state-backed vaccines will be covered without cost barriers. Pharmacies like CVS and Walgreens are already preparing to expand appointment availability across Massachusetts.
For insurers, however, the move may increase costs and administrative complexity. Insurers must now adapt to state mandates even when they differ from national standards. Over time, this may prompt wider discussions on how state vs. federal health authority should be balanced in the U.S.
Conclusion
Massachusetts’ decision to mandate insurance coverage for state-backed vaccines represents a historic shift in U.S. vaccine policy, one that prioritizes state-level autonomy over federal uniformity. By ensuring access to essential vaccines regardless of CDC recommendations, the state is addressing both public health needs and political uncertainties in the nation’s health landscape.
The move also reflects broader regional trends, with states either forming alliances or rejecting federal guidance entirely. As Massachusetts takes a leadership role in the Northeast, it signals that states are prepared to shape vaccine access based on local evidence and priorities.
At its core, the order aims to eliminate insurance barriers and ensure residents—especially vulnerable groups—continue receiving critical protection against infectious diseases. Whether other states will follow Massachusetts’ lead remains to be seen, but the decision is already setting a precedent for a more decentralized public health model.
For Massachusetts families, the immediate effect is reassurance: vaccines backed by their state will be covered, no matter the federal stance. In a time of uncertainty, that stability could prove invaluable.
Also read: Tesla Model Y Performance Review: 460bhp, Supercar Pace, and Cutting-Edge Design
FAQs of Massachusetts Orders Insurers
1. What exactly does Massachusetts’ new vaccine order mean?
It means that all health insurers in Massachusetts must cover vaccines approved by the state health department, even if they are not backed by the CDC’s advisory panel. This ensures residents won’t face out-of-pocket costs due to changes in federal vaccine guidance.
2. Which vaccines are included under the order?
The order applies to any vaccine endorsed by the Massachusetts Department of Public Health, including COVID-19 vaccines for residents aged five and older. The department will also determine which routine vaccines pharmacists can administer.
3. How does this differ from standard U.S. insurance coverage?
Typically, insurers rely on CDC recommendations to decide coverage. Massachusetts is the first state to override that system, creating a state-driven model of guaranteed coverage.
4. Will residents need to do anything to benefit from this policy?
No. Coverage will be automatic as long as the vaccine is backed by the Massachusetts health department. Residents may still need to check with providers for appointment availability, but insurance costs will be covered.
5. Could other states adopt similar measures?
Yes. Already, states like California, Oregon, Washington, Hawaii, and Colorado have taken steps to strengthen vaccine access independently. Massachusetts’ move may encourage more states to adopt state-specific vaccine mandates if federal policies remain restrictive.





1 thought on “Massachusetts Orders Insurers to Cover State-Backed Vaccines, Even Without CDC Support”